Mother searches for answers after public health says unsterile needles used at Ontario clinic
By Canadian Press on September 22, 2025.
TORONTO — Christine Lavalle feels like she’s trapped in a nightmare.
She found out on social media last week that her child might have been exposed to blood-borne infections at a Burlington walk-in clinic after public health identified the use of unsterile needles over the span of more than six years.
“How did this happen?” she said.
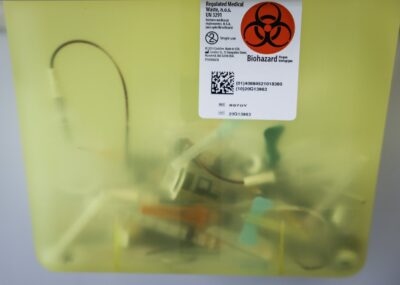
That’s the question plaguing some patients who visited Halton Family Health Centre Walk-in Clinic between Jan. 1, 2019 and July 17, 2025, and learned on Wednesday that if they received local anesthesia, they could have been exposed to hepatitis B, hepatitis C and HIV.
Halton Region Public Health said that accounts for approximately 1,000 patients.
Last spring, Lavalle said she took her child to the walk-in with a forehead gash after an incident on the playground.
She said they were seen within half an hour — a doctor froze her child’s forehead and put in two stitches. Lavalle remembers feeling relieved that she didn’t need to visit the emergency room.
But that relief turned into regret last week when she found out through a community Facebook group that Halton public health issued a notice saying it identified “improper infection prevention and control practices involving the use of unsterile needles with multi-dose vials of local anesthetic medication.” She said she was never formally notified by public health.
As she waits for more information, she’s written her questions down on a sticky note: How had this been going on for six years? Are these places not being regularly inspected? What are the consequences? How can I be assured that something like this isn’t going to happen again?
Halton Region Public Health’s medical officer of health, Dr. Deepika Lobo, said they received a complaint about the clinic on July 10 and launched an investigation that day. The public health unit does not routinely inspect medical offices, according to its website. Inspectors visit a clinic if either a complaint is filed or for a reportable disease investigation.
The College of Physicians and Surgeons of Ontario (CPSO) would not say if it is also launching an investigation, but said it is aware of concerns raised by the public health unit. The CPSO only investigates if a formal complaint is submitted, or to inspect professional misconduct and incompetency.
The public health unit recommended patients who received local anesthesia for stitches, IUD insertions, skin biopsies, removing lumps and joint injections in the time period identified get tested for blood-borne infections. Though Lobo said the risk of transmission is low, she said patients who may have been exposed should get tested as a precautionary measure.
Dr. Dick Zoutman, who teaches infectious disease control at Queen’s University, said this situation likely could have been prevented if the clinic used single-use vials instead of the cheaper multi-doses.
Zoutman said lapses can result more easily with multi-use vials, a bottle of medicine with more than one dose inside that can be used several times.
If a health provider sees a patient who needs more anesthesia and then reinserts the original needle or syringe into the vial, cross-contamination can happen if that vial is later used for another patient, he said.
“That’s the risk of using multi-dose vials … it’s just inviting trouble,” Zoutman said.
The public health unit did not go into detail about what happened, but said more broadly that staff did not follow proper infection control practices and as a result, “the anesthetic medication in multi-dose vials may have been contaminated with blood, and blood-borne infections such as hepatitis B, hepatitis C, and HIV, potentially infecting another person when the multi-dose vials were used again.”
Public Health Ontario’s infection prevention and control guidance states single-use vials are always preferred, and that multi-dose vials increase the risk of blood-borne transmission.
“Patient safety should be prioritized over cost when choosing between multi-dose and single-use medication vials,” the guidance states.
Halton Family Health Centre Walk-in Clinic did not respond to a request for comment.
Soon after Lavalle learned about the reported lapse, she picked up her kid early from school to get a blood test. She was told she would get results at a scheduled appointment next week, and pleaded to get them as soon as possible.
As she waits for the results, she’s been searching for answers, calling her doctor, the Burlington clinic, public health and the College of Physicians and Surgeons of Ontario. But she said each health provider has passed the buck to the next.
During this period of uncertainty, she said she can’t sleep through the night. The worst case scenario jolts her awake: What if her child is infected?
“Why couldn’t it be me?”
This report by The Canadian Press was first published Sept. 22, 2025.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
Hannah Alberga, The Canadian Press
30-29